Eliminating Prior Authorization Delays: Boosting Efficiency in Physical Therapy Billing
Prior authorizations are a major source of concern in the complex field of physical therapy billing. Obtaining prior authorization is similar to traversing a convoluted web of regulations; it can cause delays, rejections, and time wastage. These delays not just interrupt patient care but also stress the financial management of your practice.
Table of Contents
Examining the Deeper Issues of Prior Authorization Delays: Understanding the Pain
Requirements for prior authorization might have unintended consequences that impacts patients, therapists, and the practice’s bottom line.
For Patients:
Negative consequences may follow one another if prior authorization is not received promptly.
Treatment that is postponed or cancelled: Patients may have to wait weeks or even months to begin their physical therapy regimen. This can lead to:
- Health Deterioration: Patients who already have health problems may experience more discomfort, immobility, and difficulty doing daily activities if treatment is delayed.
2. Decreased motivation: Over time, patients may feel less motivated and enthusiastic, which may make it more difficult for them to fully recover.
3. Discontent and annoyance: Due to bureaucratic obstacles, the healthcare system may cause patients and therapists to feel dissatisfied and irritated.
For Therapists:
Patients are not the only ones burdened by prior authorizations. Therapists frequently encounter:
- Administrative Overload: Time lost on obtaining paperwork, making requests, and corresponding with insurance companies takes away from time better spent interacting with patients.
- Increased stress levels: Psychologist burnout could worsen due to the uncertainty and frustration related to the prior authorization process.
- Tense Patient Relationships: Patients may experience irritation due to delays, impacting their relationship with their therapist.
For the Practice:
Practice can suffer significant financial consequences due to delays in obtaining prior authorization.
- Decreased income: Uncompensated services stem from previous authorizations that were denied. Repayment delays can strain cash flow and make it challenging to control operating costs.
- Potential Patient Reduction: If patients are unable to get treatment quickly, they may look for alternatives elsewhere, which could have an effect on the practice’s patient base.
- Adverse Impact on Reputation: Attracting new patients may prove challenging if delays lead to negative patient feedback and damage to the reputation.
Practolytics: Your Knight in Shining Armor Against Prior Authorization Delays
At Practolytics, we understand the complexities of prior authorizations and are committed to helping physical therapy practices conquer this challenge. Here’s how we equip you for success:
Insurance Expertise: A Deep Dive- Our team isn’t just familiar with prior authorization requirements; we’re experts. We delve into the ever-changing landscape of payer rules and regulations, including:
- Comprehending Medical Necessity Criteria: We keep up to date on the particular standards that every insurance provider employs in order to establish the medical necessity of physical therapy services. This enables us to customise your authorization requests to satisfy the particular needs of every payer.
- Interpreting Insurance Manuals: Insurance guides may be intricate and perplexing. We ensure that your requests are made accurately and fully from the outset by translating the complicated terminology into manageable steps.
- Remaining Up to Date with Policy Changes: Insurance policies, like everything else in the healthcare industry, are subject to ongoing change. We notify you of any changes in prior authorization requirements that we proactively monitor.
Clear and Concise Documentation: The Cornerstone of Success Incomplete or inaccurate documentation is a major reason for prior authorization denials. Practolytics tackles this challenge by:
- Collaborative Approach: We collaborate closely with your therapists to make sure that all necessary paperwork is obtained up front, including doctor references, thorough diagnoses, and treatment plans.
- Strict Review Process: Before submitting any paperwork, our staff carefully checks it for accuracy and completeness. By doing this, the possibility of requests being returned for incomplete information is reduced.
- Standardisation and Templates: To ensure consistency and lower mistake rates, we provide standardised templates and processes for documentation.
Proactive Communication and Follow-up: Keeping the Momentum Going – We don’t just submit requests and hope for the best. Our team takes a proactive approach to ensure your requests are processed efficiently:
- Frequent Status Checks: We follow up on the status of your authorization requests by keeping in constant contact with insurance companies. This tenacious attitude minimizes delays and keeps your requests going ahead.
- Dealing with Obstacles Head-on: We make a concerted effort to identify and resolve any obstacles that arise during the process. This proactive strategy guarantees quick approvals and avoids delays.
- Expertise in Appeal: When faced with a denial, we persevere. Our staff is skilled at creating persuasive appeals that answer the grounds for rejection and provide solid evidence for the services that are being sought.
Technology: Your Trusted Toolkit for Prior Authorization Success
Practolytics utilizes cutting-edge technology to help you overcome obstacles with prior authorizations.
- Safe Digital Platform: Ask for permission online to speed up the process. This creates a trustworthy record of transactions and eliminates the time delays associated with mailing or faxing documents.
- Real-Time Monitoring: Keep track of the status of your permission requests in real-time. Through our system’s central dashboard, you have the ability to monitor updates, identify potential challenges, and respond accordingly.
- Automated Alerts and Reminders: Our system creates alerts and reminders automatically to ensure timely submission of all necessary paperwork. Alerts can be set up to notify you of any issues with your requests, allowing you to act proactively.
Empowering Physical Therapists with the Ability to Make a Difference!
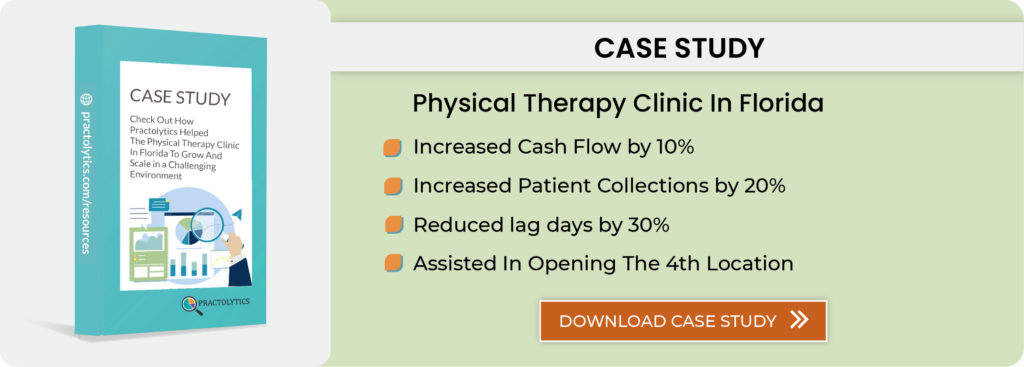
ABC Physical Therapy was struggling with a flood of prior authorization denials and delays. These challenges were leading to frustration among their patients and affecting their financial performance. Ever since teaming up with Practolytics, ABC Physical Therapy has undergone a remarkable transformation.
- 75% Decrease in Denial Rates: Thanks to Practolytics’s expertise in navigating prior authorization rules, ABC Physical Therapy has experienced a significant decrease in denied claims. The time and money lost on appeals will go down as a result of this.
- Increased Patient Satisfaction: Faster approval of authorizations enables patients to receive care promptly, reducing frustration and elevating satisfaction levels. Therapists can focus on delivering exceptional patient care without having to deal with the administrative burden of getting prior authorization.
- Increased Revenue: Speedy approvals lead to faster reimbursement, boosting ABC Physical Therapy’s cash flow and stability. They can then invest in their practice and improve patient service.
Conclusion
Prior authorization delays may have detrimental effects on patients as well as physical therapists.
Practolytics provides a thorough answer to this issue by merging human knowledge with technological resources to guarantee a more efficient prior authorization procedure. Working with Practolytics can help you streamline your practice’s financial operations, provide your patients with timely access to essential care, and focus on providing excellent physical therapy services.
Never let prior authorizations get in the way of your practice’s income or patient care.
Collaborate with Practolytics to simplify the process and guarantee timely care for your patients.
It is possible to significantly reduce delays, denials, and ensure a more efficient pre authorization process by making use of Practolytics’ expertise and solutions. This allows you to focus on what matters most: giving your community’s patients the best care possible.
ALSO READ – What Makes Outsourcing the Best Method for Prior Authorizations?
Talk to Medical Billing Expert Today — Get a Free Demo Now!