Don’t Let Denials Drain Your Revenue: Practolytics’ Approach to Denial Management in Physical Therapy Billing
Discover Practolytics’ proactive approach to denial management in physical therapy billing. We optimize claims processing, reduce denials, and maximize reimbursements.
Denied claims can be a frustrating and costly reality for physical therapy practices. A recent industry report shows that physical therapists face an average denial rate of 12.3%. This translates to a substantial loss of income, especially for smaller practices. Delays in resolving denials further exacerbate the problem, hindering your cash flow and making it difficult to manage your finances. Here at Practolytics, we understand the financial strain denials can cause. That’s why we offer a comprehensive denial management program designed to shield your practice from these preventable losses.
Table of Contents
The High Cost of Denials in Physical Therapy Billing
Claim denials can significantly impact your revenue. According to a recent industry report, physical therapists see an average denial rate of 12.3%. This translates to a substantial loss of income, especially for smaller practices. Delays in resolving denials further exacerbate the problem, hindering your cash flow and making it difficult to manage your finances.
Understanding the Reasons Behind Denials
There are various reasons why claims might be denied. Here are some of the most common culprits:
- Coding Errors: Inaccurate or missing CPT codes can lead to automatic claim denials.
- Missing or Incomplete Information: Incomplete patient information, missing prior authorizations, or inadequate medical necessity documentation can trigger denials.
- Payer Policy Issues: Each insurance provider has its own set of rules and regulations. Failure to adhere to these guidelines can result in denials.
Beyond the Basics: Additional Reasons for Physical Therapy Denials
While the above reasons are common, physical therapy practices face unique challenges when it comes to denials. Here are some additional factors to consider:
- Bundled Services: Insurance companies may deny claims for services they consider bundled together. Understanding these policies and proper coding techniques is crucial to avoid denials.
- Medical Necessity: Justification for physical therapy services is essential. Documentation that clearly outlines the medical necessity of the treatment plan strengthens your claim and reduces the risk of denial.
- Level of Care: Insurers determine the appropriate level of care based on the complexity of the patient’s condition. Coding that doesn’t align with the level of care provided can lead to denials.
- Timely Filing: Insurers have strict deadlines for submitting claims. Claims submitted past the deadline are automatically denied.
Tips for Denial Prevention: Empowering Your Physical Therapy Practice
We’ve shown that physical therapy practices may face severe financial hardships as a result of claim denials. There are proactive measures you can take to reduce denials in the first place, even though Practolytics provides a complete solution for denial management and recovery. The following useful advice will strengthen your practice:
Strengthen Your Documentation Practices:
- Detailed and Accurate Notes: Ensure your therapists document patient encounters thoroughly, including the presenting condition, objective findings, treatment plan, and progress notes. Clear documentation strengthens the medical necessity for your services and reduces the risk of denials based on insufficient information.
- Focus on Medical Necessity: Document the specific reasons why physical therapy is necessary for the patient’s condition. Use clear and concise language that aligns with the payer’s definition of medical necessity.
- Level of Care Justification: Clearly document the complexity of the patient’s condition and the level of care required. Coding should reflect the intensity and duration of the treatment sessions.
Stay Up-to-Date on Coding:
- Invest in Ongoing Training:The world of medical coding is constantly evolving. Encourage your therapists and billing staff to participate in regular training programs to stay abreast of the latest CPT codes (specifically the 2024 CPT manual) and physical therapy specific coding guidelines.
- Reliable Coding Resources:Utilize trusted coding resources such as the latest CPT manual and payer-specific coding guidelines. Practolytics can also be a valuable resource, keeping you informed of coding updates relevant to physical therapy.
Embrace Internal Audits:
- Regular Reviews: Conduct regular audits of your billing processes to identify potential errors or areas for improvement. This proactive approach can help you catch mistakes before they lead to denials.
- Focus on Areas Prone to Errors: Pay close attention to areas with a higher risk of errors, such as coding accuracy, missing documentation, or timely filing.
- Corrective Action Plans: Once you identify areas for improvement, implement corrective action plans to address the issues and prevent future denials.
Practolytics: Your Partner in Denial Prevention and Recovery
At Practolytics, we take a proactive approach to denial management. Here’s how we help you:
- Expert Coding and Claim Scrubbing: Our team of certified coders ensures your claims are submitted accurately and completely, minimizing the risk of errors. We stay up-to-date on the latest coding guidelines and address specific physical therapy bundling rules.
- Proactive Denial Prevention: We stay up-to-date on payer policies and identify potential denial red flags before they occur. Our team analyzes your documentation to ensure it clearly establishes medical necessity and aligns with the level of care provided.
- Robust Appeals Process: In the case of a denial, our experienced team handles the appeals process efficiently, following up with payers to ensure you receive the reimbursement you deserve. We understand the intricacies of physical therapy appeals and leverage our expertise to advocate for your practice.
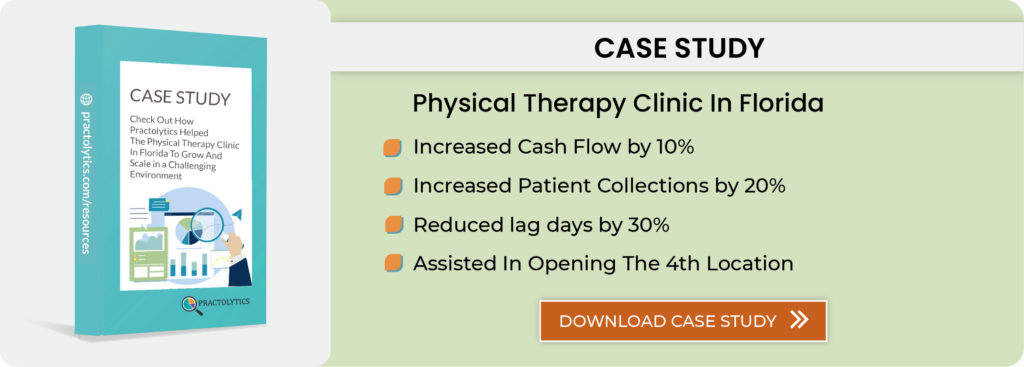
Success Stories: Practolytics Recovers Denied Claims for Physical Therapy Practices
We’re proud of our track record in helping physical therapy practices recover denied claims. Here’s an example:
- Case Study: ABC Physical Therapy was facing a significant number of denials due to incorrect coding and inadequate medical necessity documentation. After partnering with Practolytics, their denial rate dropped by 50%. Our team also successfully recovered $25,000 in denied claims, specifically focusing on appeals related to bundled services and level of care discrepancies.
Free Denial Risk Assessment for Your Physical Therapy Practice
We understand that every practice is unique. To help you identify areas for improvement, Practolytics offers a free denial risk assessment. Our experts will analyse your billing practices and pinpoint potential weaknesses that could lead to denials, including those specific to physical therapy.
Don’t let denials chip away at your hard-earned revenue. Partner with Practolytics to ensure your claims are processed accurately and efficiently. Contact us today to schedule your free denial risk assessment and learn more about our proven approach to denial management.
By implementing Practolytics’ denial management strategies, you can significantly reduce denials, improve your cash flow, and focus on what matters most – delivering exceptional patient care.
ALSO READ – Billing Guidelines Every Physical Therapist Should Know for Error-Free Claims
Talk to Medical Billing Expert Today — Get a Free Demo Now!