Effective RCM for Physical Therapy Practices to Maximize Revenue
In the field of physical therapy, timely and precise claim submission is essential to your company’s financial stability. Erroneous or delayed claims can negatively impact cash flow and put strain on your financial resources. At Practolytics, we are well aware of circumstances and for this reason, we provide a thorough claim cleansing and filing procedure that is intended to guarantee your claims are handled accurately and quickly.
Table of Contents
The High Cost of Physical Therapy Claim Errors
Even minor errors on a physical therapy claim can lead to delays or denials. These are a few typical offenders:
- Coding errors: Missing modifiers or incorrect CPT codes may result in automatic denials.
- Missing Information: Defective medical necessity documentation, absent prior authorizations, or incomplete patient demographic data can lead to claim denials.
- Inaccurate Payer Information: Submitting claims to the wrong insurance company typically leads to denial due to inaccurate payer information.
These mistakes not just consume precious time and resources in fixing them, but also prolong the reimbursement process and impede the cash flow. A new industry study indicates that physical therapists encounter an average rejection rate of 12.3%. This results in a significant decrease in revenue, particularly for smaller businesses. Delays in addressing rejections only worsen the issue, causing obstacles in your revenue flow and complicating financial management.
Preventing Errors in Physical Therapy Billing: Practical Tips to Stop Leaks in Claim Submissions
Physical therapy practices are always concerned about claim denials. Mistakes in submitting claims cannot just hold up reimbursements but also erode your profits that you worked hard for. Fortunately, a large number of these mistakes can be avoided. Below are some useful recommendations and top methods to strengthen your claim submission procedure:
Accept the Importance of Conducting Routine Audits:
Organize internal evaluations: Identify problems before relying on external audits. By regularly examining your internal billing procedures, you can identify issues in advance and detect errors before they lead to rejections.
• Focus on High-Risk Areas: Direct your audits towards areas where errors are more prone to happen, such as timely filing, incomplete data, and precise coding.
• Strategies for Rectification: Develop and execute plans for rectifying errors and preventing future occurrences of the same mistakes.
Invest in Staff Training and Education:
Coding Expertise: Make sure your billing personnel and therapists have a solid understanding of the codes that are unique to physical therapy. In order to remain current with CPT codes and revisions, it is recommended that individuals regularly participate in coding training programs.
Proper Documentation: To prove medical necessity and prevent denials, accurate documentation is essential. Give your therapists thorough training in documenting the patient’s condition, test results, treatment plan, and progress notes for every appointment.
Familiarity with Payer Policies: Each insurance company follows its own particular rules and regulations. Provide payer-specific policy training to your employees to guarantee that claims meet their unique needs.
Harness the Power of Technology:
• Electronic Health Records (EHR): Transfer patient data from the point of care to billing with ease by implementing an integrated EHR system. This reduces human data input errors, which are frequently the reason why claims are denied.
• Claim Scrubbing Software: Prior to submission, make an investment in dependable software that can find possible coding errors and missing data.
• Eligibility Verification Tools: Make sure the services provided to patients are in line with the coverage plan and that their benefits are active by using real-time eligibility verification tools. This preemptive measure aids in avoiding rejections based on ineligibility.
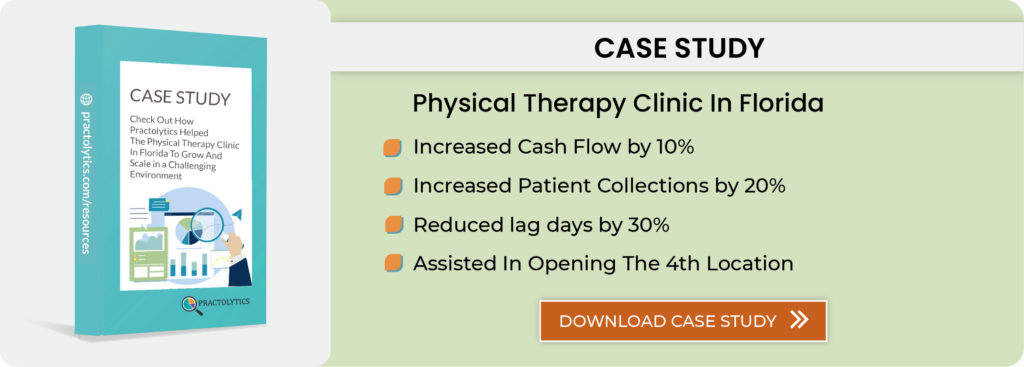
Streamlining Your Physical Therapy Claim Submission Process with Practolytics
Practolytics offers a robust solution to eliminate these errors and ensure your claims are submitted accurately and on time. Here’s what sets us apart:
• Careful Claim Scrubbing: Before submitting your claims, our team of billing specialists carefully examines them to find and fix any coding problems, missing information, or payer data.
• Thorough Documentation Review: To make sure your documentation amply demonstrates medical necessity; we go above and beyond simple coding. This lowers the possibility of rejections due to inadequate explanation for provided services.
• Simplified Submission Process: We use safe electronic submission techniques to make sure your claims are promptly and effectively received by the appropriate payer.
Technology for Accuracy and Efficiency
Practolytics utilizes advanced technology to optimize our claim scrubbing and submission process. Our secure platform integrates with your existing practice management system, allowing for seamless data transfer and minimizing manual data entry errors. Additionally, we leverage:
• Automated Coding Compliance Checks: Our software checks automatically to make sure your coding complies with payer-specific regulations and the most recent CPT guidelines.
• Real-Time Eligibility Verification: By confirming a patient’s eligibility and benefits with the majority of major payers quickly, we can reduce the possibility that claims for services that are not eligible may be submitted to the incorrect plan.
• Denial Prevention Tools: By spotting any red flags before to submission, our sophisticated analytics enable us to take proactive measures to resolve problems and stop rejections before they start.
Conquer Claim Denials in Your Style
While these tips provide a strong foundation, partnering with Practolytics elevates your claim submission process to a whole new level. With years of experience and state-of-the-art technology, our team of experts ensures that your physical therapy claims are handled with precision and speed.
Reach out to us to learn more about how Practolytics can help you:
- Reduce claim denials and improve cash flow.
- Minimize errors with our meticulous claim scrubbing process.
- Stay up to date on coding and payer rules.
- Benefit from our advanced technology solutions.
You can boost payments, lower rejections, and expedite the claim submission process by utilizing Practolytics’ technology and experience. This frees you up to concentrate just on providing outstanding patient care, which is what matters most.
ALSO READ – Navigating the Basics of Physical Therapy Billing
Talk to Medical Billing Expert Today — Get a Free Demo Now!