General Coding Guidelines for ICD-10-CM
We know coding can feel like a headache sometimes. That’s why at Practolytics, we break down the General Coding Guidelines for ICD-10-CM in a way that actually makes sense. These guidelines help you turn patient notes into accurate codes that insurers understand. When your documentation is clear, claims get approved faster, denials drop, and your revenue cycle feels a lot smoother. In this blog, we’ll walk you through the essentials, point out common mistakes we see in real clinics, and show how our team helps providers put these rules into practice without all the stress.
Let’s be honest—most providers didn’t get into healthcare to spend their days thinking about coding rules. You trained to treat patients, not to worry about whether an insurer prefers an Excludes1 note or a laterality detail. And yet, if your documentation doesn’t line up with the General Coding Guidelines for ICD-10-CM, your claims may get denied. That denial doesn’t just frustrate your staff; it delays your payment, stresses your patients, and slows down your entire practice.
That’s where these guidelines come in. They’re essentially the map that helps us translate what happens in the exam room into the language payers understand. Without the map, you’re guessing—and in healthcare, guessing can be expensive.
At Practolytics, we’ve seen firsthand how following (or ignoring) these guidelines impacts financial outcomes. One practice we worked with was losing thousands every month because their physicians weren’t documenting laterality on orthopedic injuries. Simple detail, big loss. Once we trained their team on these ICD-10-CM coding principles for beginners, denials dropped, revenue improved, and stress levels eased.
That’s why we’re so passionate about this topic—because getting coding right doesn’t just help with compliance, it keeps practices financially healthy.
Table of Contents
Structure of ICD-10-CM
Before we dive into the rules, let’s talk structure. The ICD-10-CM coding conventions aren’t random; they’re carefully organized to capture clinical detail.
- Character 1: Always a letter, showing the chapter/category (like “C” for cancers or “M” for musculoskeletal).
- Characters 2–3: Narrow down the condition (for instance, knee vs shoulder within musculoskeletal).
- Characters 4–6: Add details like severity, location, or laterality.
- Character 7: Extender—for encounter type (initial, subsequent, or sequela).
Think of it like building a patient’s story, one character at a time. The code doesn’t just say “broken bone.” It says “right tibia fracture, initial encounter, displaced.” That detail matters. It matters for clinical accuracy, but also for payers who won’t reimburse unless the story is complete.
And here’s the kicker: if you don’t document those details, coders can’t invent them. Missing laterality? Missing chronicity? They’re forced to use an unspecified code, which insurers hate. That’s why we stress training on how to apply ICD-10-CM conventions across your entire team—not just coders, but physicians and nurses, too.
Reasons For General Coding Guidelines
So, why do we have all these rules? At first glance, they may feel like red tape. But there’s a real purpose behind them:
- Consistency across providers: Whether you’re coding in New York or Nashville, the same rules apply.
- Accuracy in patient stories: Codes aren’t just for billing—they’re used in research, public health tracking, and quality reporting.
- Compliance with payers and regulators: Following the ICD-10-CM official guideline overview keeps you audit-ready and reduces risk.
Here’s how we explain it to clients: coding guidelines are like seatbelts. They might feel restrictive at times, but they protect you from much bigger problems down the road.
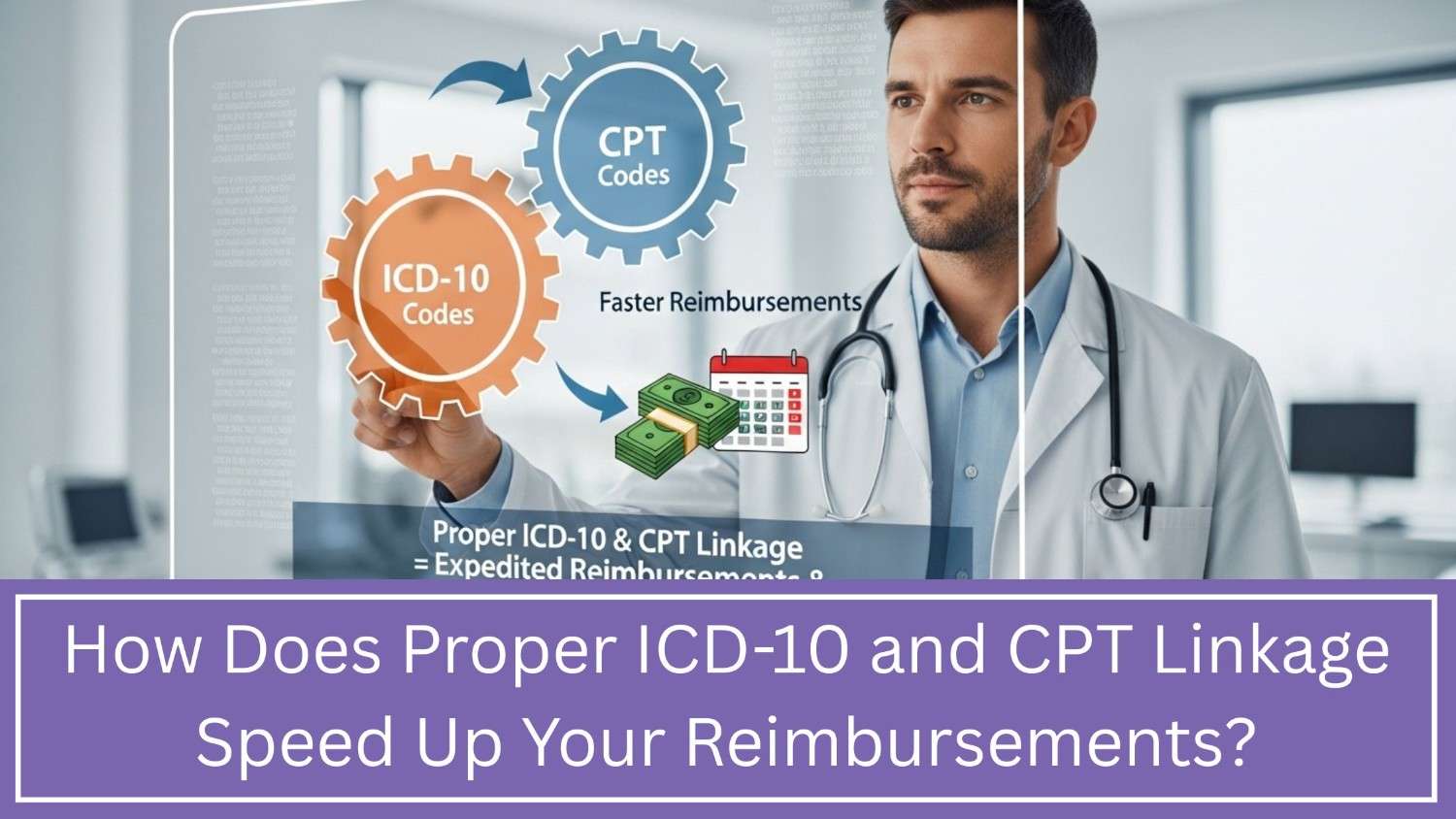
Procedure for Code Selection
Choosing the right code isn’t just about flipping open a book (or scrolling through your EMR’s code search). It’s a deliberate process. Here’s how we walk coders through it:
- Identify the main term: What’s the condition? Pneumonia? Diabetes? Knee injury?
- Check the Alphabetic Index: Find the code range.
- Verify in the Tabular List: Always confirm details in the official list—not just the index.
- Follow conventions: If there’s a “code first” instruction, you can’t ignore it. If there’s a “use additional code,” don’t skip it.
- Capture specificity: Laterality, chronic vs acute, initial vs subsequent visit.
- Review sequencing: Primary condition first, secondary conditions after.
Skipping steps creates errors, and errors lead to denials. We’ve had providers ask, “Why is my chronic kidney disease claim being denied?” The answer often lies in step 4—they ignored the “code first diabetes” instruction. Once we aligned their workflow with ICD-10-CM guideline tips and best practices, the problem disappeared.
Acute and Chronic Conditions
This is one of the trickiest areas for physicians. Many conditions can be both acute and chronic, and ICD-10-CM expects you to document both if applicable.
Example:
- Chronic asthma with an acute flare-up.
- Chronic heart disease with an acute myocardial infarction.
Both should be coded if present. If you only document “asthma” or “heart condition,” the story is incomplete. That not only confuses coders, but it risks underpayment.
Our tip: Be explicit. If it’s acute, say so. If it’s chronic, document it. If it’s both, write both. This makes it easier for coders to apply the right ICD-10-CM coding rules and guidelines, and it ensures insurers reimburse you for the actual complexity of care.
Common Errors in Chapter-Specific Guidelines
Let’s talk about the elephants in the room—common mistakes we see all the time:
- Mixing up Excludes1 and Excludes2 notes: Excludes1 = you can’t code both. Excludes2 = you can code both if present. Huge difference.
- Skipping laterality: Writing “fractured arm” without noting right or left. (Insurers will deny.)
- Ignoring “Code First” rules: For example, diabetic neuropathy must be coded with diabetes first, not neuropathy first.
- Overusing unspecified codes: It’s tempting when documentation is thin, but insurers see it as sloppy.
At Practolytics, we don’t just point out errors—we help fix them. That means training physicians to document better, auditing coding for accuracy, and coaching staff so these mistakes become rare.
How This Ties Into Revenue Cycle Management?
Here’s where it all comes together. You might be thinking, “Okay, coding guidelines are important—but what does this have to do with my revenue?”
The answer: everything.
When coding is clean and compliant:
- Claims go through on the first pass (we average 97% first-pass ratio).
- Denials drop, which means less staff time wasted.
- Payments arrive faster, smoothing out cash flow.
When coding is sloppy:
- Denials stack up.
- Revenue leaks out.
- Providers get frustrated, patients get confused, and staff burn out.
That’s why coding support is baked into our end-to-end healthcare revenue cycle management services. We don’t just manage billing—we actively coach providers on documentation, run proactive audits, and apply predictive analytics to catch errors before they turn into denials.
One of our orthopedic clients cut denials by 40% within three months of working with us, simply by improving laterality documentation. That’s the power of combining ICD-10-CM chapter guideline rules with smart revenue cycle processes.
Practolytics: Your Partner in Coding and Revenue!
With more than two decades in this space, we’ve seen it all—small practices struggling with denials, large groups drowning in backlogs, specialists frustrated by coding quirks. Our job is to make all of that easier.
Here’s what we bring to the table:
- Deep knowledge of ICD-10-CM coding conventions.
- Training for providers and staff on how to apply ICD-10-CM conventions in real life.
- Real-time analytics that show you where errors (and revenue leaks) are happening.
- Proven workflows that cut claim submission time from 15 days to 7 days.
At the end of the day, our promise is simple: you focus on patients, we’ll focus on getting you paid accurately and on time.
Conclusion:
We know—General Coding Guidelines for ICD-10-CM can feel tricky at first. But really, it’s all about telling your patient’s story clearly. When your notes are clear, claims go through faster, denials drop, and your revenue cycle runs smoother.
By avoiding common mistakes, documenting carefully, and having a partner like us, coding doesn’t have to be stressful. It’s not just about rules—it’s about helping you focus on what you do best: taking care of patients, while we help keep your practice financially healthy.
Get your documentation right, and everything else—claims, payments, revenue—falls into place. That’s the Practolytics promise.
What is the most important thing as a physician, must change in my documentation to support ICD-10-CM?
Specificity. Always be specific—laterality, chronic vs acute, complications, and cause. Vague notes create vague codes, and vague codes get denied.
How do I document for laterality (right/left/bilateral) for conditions like joint pain or injuries?
Write it exactly—“right knee pain,” “left wrist fracture,” or “bilateral hip arthritis.” Never assume coders can guess.
What is a “Code First” or “Use Additional Code” note, and how does it affect my primary diagnosis selection?
“Code First” means another condition should be listed before the one you’re coding. “Use Additional Code” means you should add extra detail codes. Both rules ensure the full story is captured.
What is the difference between Excludes1 and Excludes2 notes in the code set?
Excludes1 = never code the two conditions together (they can’t coexist). Excludes2 = the two conditions can coexist, so both can be coded if documented.For chronic conditions, should I document “resolved” symptoms or complications from a previous visit?
Yes—if relevant. Document both resolved symptoms and ongoing complications. This helps coders apply the right ICD-10-CM guideline tips and best practices and gives payers a complete picture.
ALSO READ – Decoding CPT: Your Guide to Codes and Regulations 2024
Talk to Medical Billing Expert Today — Get a Free Demo Now!